Ladies, have you ever experienced that uncomfortable itch or noticed a thick, white discharge? You may be wondering if it’s a yeast infection, and if so, what can be done to treat and prevent it. In this article, we will explore everything you need to know about vulvovaginal candidiasis (VVC), also known as vaginal thrush. We’ll cover its symptoms, risk factors, prevention strategies, debunking myths and misconceptions, related conditions, and treatment options. We hope to provide you with the information you need to manage this common and easily treatable infection.
What is candidiasis?
Candidiasis is a fungal infection caused by yeasts from the family candida, which is the most common fungus to affect humans. The commonest type is candida albicans. Candida can be found in the gastrointestinal, genitourinary and respiratory tracts. In more severe cases, candida infection can be invasive and affect the whole body.
The focus of my article is on vulvovaginal candidiasis (VVC) also more commonly known as vaginal thrush. VVC is very common in women, with about ¾ of women experiencing an episode of this during their lifetime and is the second most common cause of vaginitis in women.
Approximately 5% of women experience recurrent attacks of VVC which is defined as ≥ 4 infection per year.
Symptoms of vulvovaginal candidiasis (VVC):

*Vulva refers to the external genetelia of the female, including the labia majora, labia minora, clitoris and vestibule of the vagina.
- Red swollen vagina and labia
- Severe vulva itch (pruritus)
- Vaginal discharge – thick, white, curdlike, ‘cottage-cheese’ discharge
- Pain passing urine (dysuria)
- Pain during sex (dyspareunia)
- Irritation and pain around surrounding affected area
- Obvious thickening and swelling of skin secondary to chronic scratching (lichenification)
Risk factors:
1. Pregnancy
During pregnancy, candida infection is more common. This is due to changes in hormone levels such as oestrogen.
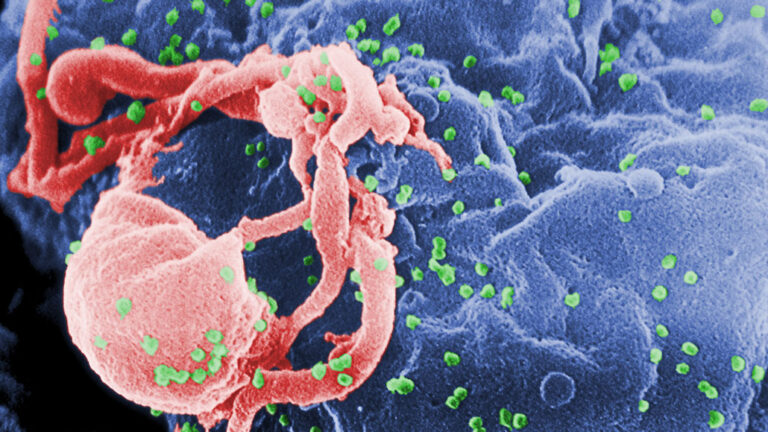
2. Immunocompromised
Such as those living with AIDS, poorly controlled diabetes mellitus and receiving chemotherapy.
This is due to the inability of the body’s immune system to effectively control the spread of the candida fungus.
3. Antibiotics usage
Antibiotics are not effective against yeast infections and they can also kill good bacteria normally found in the vagina. Once this happens there is less competition facing other infections, such as candida, which means they can flourish.
4. Lifestyle
The link between personal hygiene, tight fitting undergarments and candidiasis remains controversial.
Also, sexual activity is not related to candida infection and infections often occur without having sex.
Treatment:

Over-the-counter (OTC) medications are generally highly effective for treating candidiasis.
However, self-medication with OTC preparations should be advised only for women who have had prior diagnoses of VVC and who had recurrence of the same symptoms.
Should symptoms persist it is advised that you seek medical attention as incorrect or inappropriate treatment is common, which can lead to other vaginal infections.
If you think you could be suffering from VVC and have tried OTC preparations but are still having symptoms or if you are unsure of the symptoms you are experiencing, please see a doctor. VVC is very common in ladies and is an easily treatable infection.
Prevention Strategies:
Maintaining a healthy balance of vaginal flora: A healthy vaginal environment is essential for preventing VVC. This includes avoiding the use of douches, scented soaps, and other products that may disrupt the delicate balance of good bacteria in the vagina. Additionally, wiping from front to back after using the toilet can help prevent the introduction of harmful bacteria to the vaginal area.
Dietary recommendations: Consuming a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can contribute to overall health and may help prevent VVC. Limiting sugar intake and consuming foods containing probiotics, such as yogurt and kefir, may also help maintain a healthy balance of vaginal flora.
Probiotics and their potential benefits: Probiotics are live microorganisms that, when consumed in adequate amounts, can provide health benefits. Some studies suggest that certain probiotics may help prevent VVC by restoring the balance of good bacteria in the vagina. However, more research is needed to determine the most effective strains and doses.
Proper hygiene practices: Practicing good hygiene is essential for preventing VVC. This includes changing underwear daily, wearing breathable cotton underwear, and avoiding tight-fitting clothing that can create a warm, moist environment conducive to yeast growth.
Myths and Misconceptions about VVC:

Debunking myths about causes and transmission: Many people mistakenly believe that VVC is solely caused by poor hygiene or can be transmitted through sexual contact. While sexual activity can sometimes trigger VVC, it is not considered an STI. Additionally, VVC is not a result of poor hygiene; rather, it is caused by an overgrowth of yeast that can occur for various reasons, including hormonal changes, antibiotic use, and weakened immune systems.
Clarifying misconceptions about treatments: Some people may believe that over-the-counter (OTC) antifungal creams are the only treatment option for VVC. While OTC medications are often effective, some cases may require prescription-strength treatments or alternative therapies. It is essential to consult with a healthcare provider for accurate diagnosis and treatment recommendations.
Understanding the role of sexual activity in VVC: Although sexual activity can sometimes trigger VVC, it is not considered an STI. Couples do not need to abstain from sex when one partner has VVC; however, engaging in sexual activity during an active infection may cause discomfort and prolong the healing process.
Dispelling fears and stigma associated with VVC: Many women may feel embarrassed or ashamed when experiencing VVC symptoms. It is important to remember that VVC is a common condition that affects millions of women and is not a reflection of one’s cleanliness or sexual behavior.
Complications and Related Conditions:

Impact of untreated VVC on sexual health: If left untreated, VVC can lead to discomfort and pain during sexual activity, which can negatively impact one’s sexual health and relationships. It is crucial to seek treatment if you suspect you have VVC to prevent potential complications.
VVC and pregnancy: Pregnant women are more susceptible to VVC due to hormonal changes. Although VVC is not generally harmful to the baby, it can cause discomfort for the mother. Pregnant women should consult their healthcare provider for the safest and most effective treatment options.
Recurrent VVC: Some women may experience recurrent VVC, defined as four or more episodes per year. This can be frustrating and may require long-term treatment and management. Healthcare providers can help develop a personalized treatment plan to reduce the frequency and severity of recurrent VVC.
FAQ
Can men get VVC?
While uncommon, men can also develop VVC, although they are less likely to experience symptoms. In men, VVC can cause redness, itching, and a rash on the penis.
Can VVC be sexually transmitted?
VVC is not considered a sexually transmitted infection (STI). However, sexual activity can sometimes trigger VVC.
Can VVC affect fertility?
VVC does not typically affect fertility. However, untreated VVC can lead to discomfort and pain during sex, which can negatively impact sexual health and relationships.
Can VVC go away on its own?
Mild cases of VVC may go away on their own without treatment. However, it is recommended to seek medical attention for accurate diagnosis and treatment to prevent potential complications.
Can I still exercise with VVC?
It is generally safe to exercise with VVC. However, it is recommended to wear loose-fitting clothing and avoid activities that may cause discomfort.
Conclusion
Vulvovaginal candidiasis (VVC) is a common and easily treatable infection that affects many women. By understanding the symptoms, risk factors, prevention strategies, and treatment options, women can take control of their vaginal health and seek appropriate medical attention when necessary. It is important to dispel myths and misconceptions surrounding VVC to reduce stigma and promote accurate information sharing. Remember, VVC is not a reflection of one’s cleanliness or sexual behavior, and seeking medical attention is the best way to manage and prevent potential complications.
Related Posts:
- How Can You Charge Apple Pencil With iPhone? - Apple…
- Top 6 Myths on How You Can Get Infected with HIV
- Understanding Vaginal Discharge: What's Normal and…
- Understanding Abnormal Vaginal Bleeding: Unraveling…
- Anal Itching: Understanding the Causes and Finding Relief
- How to Increase Testicle Size - Busting Myths and…