Genital warts, a common sexually transmitted infection, can appear on your skin anywhere in the genital area. They often present as white or flesh-coloured, smooth, small bumps, or in some cases, larger, fleshy, cauliflower-like lumps. The appearance can vary greatly, and it’s not uncommon for them to go unnoticed, especially if they’re hidden within the genital region.
These warts are caused by the human papilloma virus (HPV), a complex group of viruses that can infect various parts of the body, including the skin and mucous membranes. Over 200 subtypes of HPV exist, but thankfully, the majority of these do not cause clinically significant disease. However, about 30 of these subtypes can infect the genital area, and these are the ones we need to be aware of.
Of these 30, a few can cause genital warts. It’s important to note that having genital warts doesn’t necessarily mean you’ll develop cancer. However, certain high-risk types of HPV can lead to cancer of the cervix, vulva, anus, and penis. This is why regular screenings, such as Pap smears for women, are crucial for early detection and treatment.
If you’re wondering how you can protect yourself, the good news is that there are vaccines available that can protect against the most common types of HPV that cause genital warts and cancer. It’s recommended for young people to get vaccinated, but if you missed out on the vaccine when you were younger, it might not be too late. Speak to your healthcare provider to find out more.
How do I get the disease?
The HPV virus that causes warts are transmitted through genital skin contact, or through transfer of genital fluids. You do not need penetrative sexual contact to acquire the infection. Condoms and other barrier methods provide only limited protection against HPV. In rare cases, there can be transmission through childbirth.
How do I know I am infected for HPV? How can it be detected?
Generally, HPV viruses as a group do not cause symptoms and the majority are unaware that they are infected with HPV. Nevertheless, a small group present with genital warts which are small bumps or larger fleshy, cauliflower-like lumps on the skin or mucous membranes in the genital area. They usually appear about 1 to 3 months after initial infection.
The most severe disease that HPV can cause is cervix cancer and hence, women are advised to go for pap smears with their doctors regularly.
There is a test for the high risk HPVs (amongst them 6, 11, 16, 18) which is available in certain clinics.
For MSM, it is recommended that they do the Anal Pap as well.
How can HPV be treated?
There is no specific treatment for HPV as the infection is usually self limiting. In general, the body’s immunity usually clears the infection after some time. Notwithstanding, some people have lingering infection, especially in people who’s immunity is impaired, e.g. due to concurrent infection with HIV.
For genital warts that HPV causes, treatment depends on how severe and extensive the warts are.
The most common and effective treaments are:
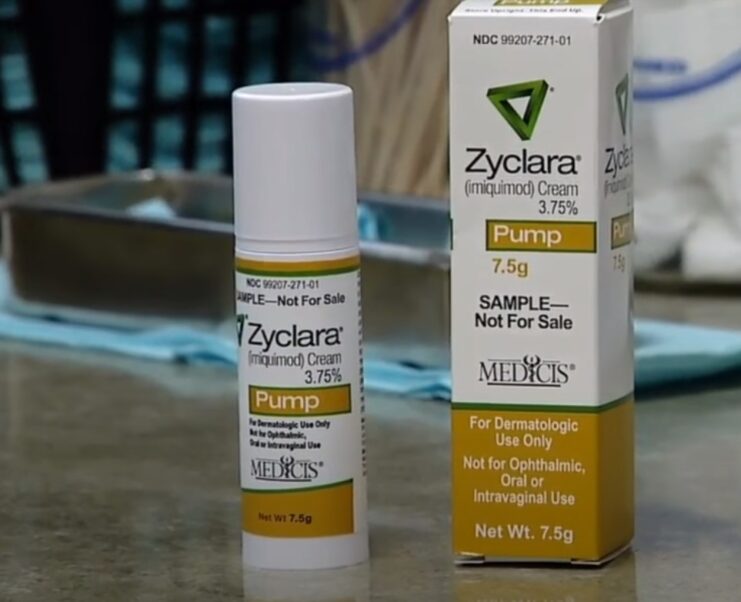
- Imiquimod cream which is marketed as an “immune modulator” which recruits the body’s immunity against the wart. They need to be applied thrice weekly and left on overnight for the best effect.
- Cryotherapy with liquid nitrogen which “freezes” the wart and destroys them.
- Electrocautery/surgical excision removes the wart surgically.
The majority of genital warts recur even after adequate treatment and repeat treatments may be needed to completely eradicate the problem.
HPV and Cervical cancer
High risk HPV viruses (especially types 16 and 18) can induce changes in the cervical cells and this can lead to cancer of the cervix. This is why all sexually active women are advised to get themselves screened for HPV and also to go for a regular Pap smear test.
Pap smear is a screening test for cervical cancer. It involves opening the vagina to take a small sample of cells from the cervix (opening of the uterus/womb) with a swab and examining those cells under a microscope. If there are any abnormal changes in these cells, the patient will be referred for further examination and treatment to eradicate the problem.
These high risk subtypes of HPV also cause changes in the anal/rectal mucosa that predisposes men and women who engage in anal intercourse to cancer. In these men or women, Anal Pap, which is available in certain clinics including clinics under the Robertson Medical Group (link) is available as a screening test.
Prevention of HPV, Cervical Cancer and Genital Warts

Theare are currently 2 vaccines available to prevent cervical cancer and genital warts caused by the major high risk subtypes of HPV. The first to be approved is Gardasil which protects against 4 high risk subtypes and is effective for genital warts and cervical cancer prevention.
The other vaccine, Cervarix protects against the 2 high risk subtypes which cause cervical cancer.
It is however, not used for prevention against genital warts.
Final Words
In conclusion, HPV and the resulting genital warts are a common and often misunderstood condition. It’s important to remember that while HPV is common, not all types of the virus lead to serious health issues like cancer. Regular screenings and vaccinations can go a long way in preventing the most severe outcomes.
The key to managing HPV and genital warts is education and prevention. Understanding how the virus is transmitted, recognizing the signs and symptoms, and knowing the available treatment options are all crucial steps in managing this condition.
Remember, there’s no shame in having HPV or genital warts. It’s a common condition that affects many people around the world. If you’re dealing with this, know that you’re not alone and there are resources and medical treatments available to help you.