Your friendly health blogger is back with another insightful post. We’re diving into a topic that’s essential for everyone who’s sexually active – contraception. It’s all about keeping things safe and sexy, so let’s get started!
Contraception, in essence, is the practice of preventing pregnancy following sexual activity. It’s a crucial aspect of sexual health, and it’s important to understand the different options available.The most common methods are barrier and hormonal contraception.
1. Barrier Contraception

Firstly, let’s talk about barrier methods. The most popular form of barrier contraception is the condom. It’s affordable, safe, and has the added advantage of reducing the risk of HIV and other sexually transmitted infections.
However, some individuals may experience itching, rashes, or other localized reactions due to allergies to latex or the lubricants and spermicides used with condoms. For such individuals, latex-free options are available. If symptoms persist or worsen, it’s always a good idea to consult your doctor.
Benefits:
- Provides immediate protection against pregnancy.
- Reduces the risk of sexually transmitted infections (STIs), including HIV.
- Does not involve hormones or any systemic side effects.
- Can be used only when needed, offering flexibility.
Side Effects:
- Some people may experience allergic reactions to latex (used in most condoms) or to the spermicides that are sometimes used with barrier methods.
- There’s a risk of breakage or slippage during intercourse.
- Requires proper usage for effective protection.
2. Hormonal Contraception
These methods work by either preventing ovulation or stopping the implantation of a fertilized egg in the womb. Hormones can be delivered in various ways – orally (pills), via injections, or through daily skin patches.
Oral contraceptives are the most widely used form of hormonal contraception. They are highly reliable when taken as directed, and fertility quickly returns once the pills are stopped. Other benefits include improvements in acne and a possible reduction in the risk for ovarian cancer.
However, like all medications, oral contraceptives can have side effects. These may include breakthrough bleeding, weight gain, nausea, breast discomfort, and headaches. While there may be small increases in blood pressure, this is usually not a concern in otherwise healthy individuals. Doctors will monitor your blood pressure periodically if you are on hormonal contraceptives.
There are a variety of different preparations for oral contraception available at our clinics. Newer oral contraceptives are generally well tolerated and have lower hormonal content compared to the first-generation pills.
However, they may not be suitable for specific groups of patients, such as those who are:
- obese smokers
- previously diagnosed with breast or gynecological cancer
- previously diagnosed with clotting disorders
- hypertensives, with poorly controlled blood pressure
- have pre-existing liver or heart conditions
Such patients should discuss other available options with their family doctor or gynecologist.
For those who may forget to take their pills or prefer greater convenience, injectable or implantable contraception may be a good option. Injectable contraceptives are administered into the buttock region within the first five days of the start of the menstrual cycle and provide reliable contraception from the second month onwards, as long as the three-monthly injections are continued. However, these injections may disrupt the menstrual cycle.
Implantable contraceptives can last up to three years. Apart from the small risk of injection site infection, the main side effects from these preparations are changes to the menstrual cycle, headaches, and mood changes.
Patch contraceptives deliver similar hormones as oral contraceptives and therefore carry similar side effects. Each skin patch lasts for one week and has to be changed twice within one menstrual cycle.
‘Emergency’ or post-coital contraception is also available. This consists of two oral pills, to be started within 72 hours of sexual intercourse, to reduce the chance of pregnancy. Possible side effects include menstrual irregularities, nausea, and vomiting.
Benefits:
- Highly effective at preventing pregnancy when used correctly.
- Can regulate menstrual cycles and reduce menstrual cramps.
- May improve acne and reduce the risk of ovarian cancer.
- Fertility is quickly restored once you stop taking them.
Side Effects:
- Can cause side effects such as weight gain, nausea, breast tenderness, and headaches.
- May cause irregular bleeding or spotting.
- Some forms (like the pill) require daily administration, which can be inconvenient for some.
- Does not protect against STIs.
- Certain health conditions may prevent some individuals from safely using hormonal contraception.
3. Other Options
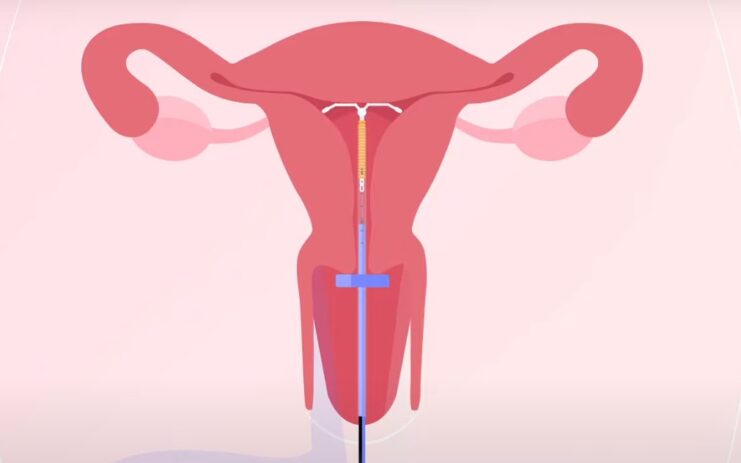
Lastly, some patients may prefer other methods of contraception, such as the insertion of an intra-uterine contraceptive device (IUCD) or Natural Family Planning methods.
Intra-Uterine Contraceptive Device
As IUCD can be a very effective and beneficial contraception method it, also has several potential side effects like everything else:
Benefits:
- Long-term, reversible contraception (can last up to 5-10 years depending on the type).
- Once inserted, you don’t have to worry about contraception on a daily basis.
- Hormonal IUCDs can reduce heavy periods.
- Fertility is quickly restored once the IUCD is removed.
Side Effects:
- Can cause side effects such as irregular bleeding, spotting, or heavier periods (especially with non-hormonal IUCDs).
- Small risk of the IUCD being expelled from the uterus or moving position.
- Does not protect against STIs.
- Rarely, the IUCD can perforate the uterus during insertion.
Natural Family Planning
Natural Family Planning, also known as fertility awareness-based methods, involves tracking your natural cycle to determine the days you are most fertile. During these fertile days, you would either abstain from sexual intercourse or use a barrier method to prevent pregnancy.
Benefits:
- Since NFP methods do not involve the use of drugs or devices, they do not have physical side effects.
- These methods do not involve ongoing costs
- Can help you become more aware of your body and its patterns, which can be useful for more than just contraception.
- Some people choose NFP methods because they align with their personal, religious, or cultural beliefs.
Side Effects:
- NFP methods are generally less effective at preventing pregnancy than some other methods of contraception. The effectiveness can vary widely, depending on how accurately the methods are practiced.
- To use NFP methods effectively, you need to accurately track your menstrual cycles and understand the signs of fertility.
- Like most other forms of contraception, NFP methods do not provide protection against sexually transmitted infections.
Remember, it’s important to discuss with your healthcare provider to determine which method is best for you, considering your health, lifestyle, and personal preferences.
FAQs
What are some alternative options if I’m allergic to latex condoms?
If you’re allergic to latex, there are latex-free condoms available. You can also consider other forms of contraception such as hormonal contraceptives or intra-uterine contraceptive devices (IUCDs).
Are there any non-hormonal contraceptive options?
Yes, barrier methods like condoms and IUCDs.
Can contraception methods help with acne?
Yes, some hormonal contraceptives can help improve acne.
What should I do if I forget to take my oral contraceptive pill?
If you forget to take your pill, take it as soon as you remember. If you missed a day, you might need to use a backup method of contraception. Always consult your healthcare provider for advice.
Can I use contraceptives even if I’m not sexually active?
Yes, some people use hormonal contraceptives for reasons other than preventing pregnancy, such as regulating menstrual cycles or reducing menstrual cramps.
Can I switch between different contraceptive methods?
Yes, but it’s important to consult your healthcare provider before switching to ensure the new method is suitable for you and to understand how to transition safely.
Can I get pregnant immediately after stopping hormonal contraceptives?
Fertility is usually restored quickly after stopping hormonal contraceptives, but it can vary from person to person.
What is emergency contraception and when should it be used?
Emergency contraception is used to prevent pregnancy after unprotected sex or contraceptive failure. It should be used within 72 hours of sexual intercourse.
Can any contraceptive method guarantee 100% protection against pregnancy?
No contraceptive method can guarantee 100% protection. Condoms offer maximum protection of 97%. (3% of the time you’re not protected – Joey Tribbiani)
Can smoking affect the effectiveness of contraceptives?
Smoking can increase the risk of certain side effects with hormonal contraceptives. It’s important to discuss your lifestyle habits with your healthcare provider when choosing a contraceptive method.
Can I use more than one contraceptive method at a time for extra protection?
Using multiple methods, like a condom and a hormonal contraceptive, can increase protection against pregnancy and STIs. However, it’s important to discuss this with your healthcare provider.
Bottom Line
Contraception is a broad field with a variety of options to suit different needs and lifestyles. It’s important to remember that what works best for one person might not work as well for another. Always consult with a healthcare provider to make an informed decision about your contraceptive method. Stay informed, stay empowered, and take control of your reproductive health.
Related Posts:
- Is Tlauncher Safe to Download? Or Not? - Make Your…
- Trichomoniasis: Diagnosis and Treatment Options for…
- Contraception After Delivery: A Comprehensive Guide
- Long Term Contraception: Embracing the Future
- Bacterial Vaginosis: Causes, Symptoms, and Treatment Options
- Ultimate Guide to Chlamydia: Diagnosis and Treatment Options