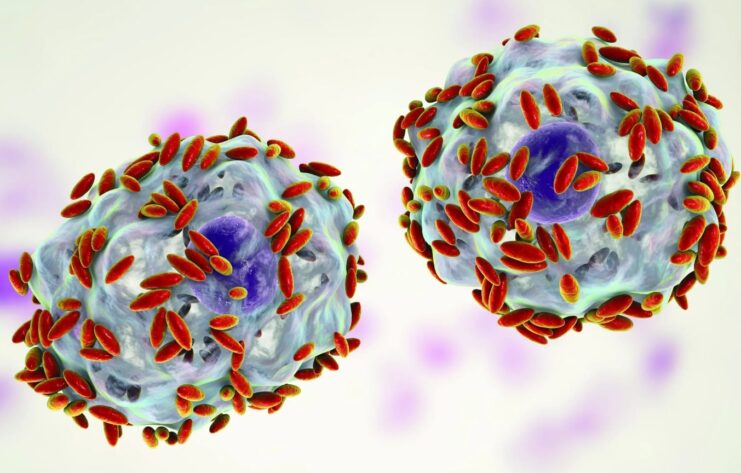
Bacterial vaginosis (BV) is a condition that results from an imbalance in the vaginal flora, which includes both “good” and “harmful” bacteria. BV is characterized by a decrease in the number of beneficial bacteria, such as Lactobacillus, and an overgrowth of harmful bacteria, including Gardnerella vaginalis.
BV is the most common cause of vulvovaginitis in women, and while it is not considered a sexually transmitted infection, it can increase the risk of contracting other sexually transmitted infections. Many women with BV do not experience symptoms, and in some cases, BV can resolve on its own without treatment.
This includes both ‘good’ and ‘harmful’ bacteria commonly found in the vagina. The bacteria commonly involved in BV are very diverse but majority involve Gardnerella vaginalis.
However, if left untreated, BV can lead to complications such as pelvic inflammatory disease and preterm birth.
Risk factors for BV:
Several factors can increase a woman’s risk of developing bacterial vaginosis (BV), including:
- New or multiple sex partners: Women who have new or multiple sex partners are more likely to develop BV. This may be due to changes in the vaginal bacteria that can occur after sexual activity.
- Douching: Douching is the practice of washing the inside of the vagina with water or other solutions. Douching can disrupt the natural balance of bacteria in the vagina and increase the risk of developing BV.
- Pregnancy: Pregnant women are at higher risk of developing BV, possibly due to hormonal changes that occur during pregnancy.
- Recent antibiotic use: Antibiotics can disrupt the natural balance of bacteria in the vagina, making it easier for harmful bacteria to grow and causing BV.
- Having an intrauterine device (IUD): Women who use an intrauterine device (IUD) for birth control may have an increased risk of developing BV, although the reason for this is unclear.
- Women who have sexually transmitted infections (STIs): Women who have certain sexually transmitted infections (STIs) may be at higher risk of developing BV, such as chlamydia and gonorrhea.
While having these risk factors can increase the likelihood of developing BV, not all women with these risk factors will develop the condition. It is important for women to be aware of the symptoms of BV and seek medical attention if they experience any signs of infection. Additionally, practicing good hygiene, avoiding douching, and using condoms during sexual activity can help reduce the risk of developing BV.
Symptoms of BV:

Many women with bacterial vaginosis (BV) do not experience any symptoms. When symptoms do occur, they may include:
- Abnormal vaginal discharge: A thin, grayish-white, or yellowish vaginal discharge is one of the hallmark symptoms of BV. The discharge may have a strong fishy odor, especially after sex.
- Vaginal odor: A strong, unpleasant odor from the vagina is a common symptom of BV. The odor may be especially noticeable after sex.
- Vaginal itching or irritation: Some women with BV may experience vaginal itching, burning, or irritation.
- Pain during urination: Some women with BV may experience pain or burning while urinating.
- Pain during sex: BV may cause pain or discomfort during sexual intercourse.
It is important to note that these symptoms can also be caused by other vaginal infections or sexually transmitted infections (STIs). Therefore, it is important to seek medical attention if you experience any of these symptoms. A healthcare provider can perform an exam and tests to determine the cause of the symptoms and recommend appropriate treatment.
Treatment:
BV will sometimes resolve without treatment.
In general, women without any symptoms of BV but who are found to have Gardnerella vaginalis colonization do not need treatment. Also, male sex partners of women diagnosed with BV do not need treatment.
Treatment is usually initiated in women with symptoms and is also especially important in pregnant ladies (with or without symptoms) as it is linked with having premature babies and babies with low birth weight.
Treatment with antibiotics either orally or vaginally is highly effective in treating BV. The use of probiotics as prophylaxis or treatment of BV remains controversial but the risk of harm is minimal.
Treatment of BV may also reduce the risk of contracting other STIs such as Chlamydia and gonorrhea, which can sometimes cause pelvic inflammatory disease (PID), causing subfertility.
As with all infections, BV can recur even after treatment. So, if you start having symptoms even after treatment, it is advisable to see your doctor for advice as you could have a recurrent infection or a STI.
Diagnosis

The diagnosis of bacterial vaginosis (BV) is typically made by a healthcare provider through a physical examination and laboratory tests. During the physical examination, the healthcare provider may collect a sample of vaginal fluid for testing.
Laboratory tests used to diagnose BV include a whiff test, wet mount test, and pH test. During the whiff test, a sample of vaginal fluid is mixed with potassium hydroxide (KOH), which can cause an odor if BV is present. The wet mount test involves examining a sample of vaginal fluid under a microscope to look for the presence of bacteria associated with BV. The pH test measures the acidity of vaginal fluid, which is typically elevated in women with BV.
In some cases, a culture test may also be performed to identify the specific bacteria causing the infection.
It is important to seek medical attention if you experience any symptoms of BV, as untreated BV can increase the risk of complications and may increase the risk of contracting sexually transmitted infections. Regular testing for sexually transmitted infections, including BV, is also important for sexually active individuals, especially those with multiple sexual partners or who engage in high-risk behaviors.
Prevention of BV
Prevention of BV involves maintaining good vaginal health and avoiding behaviors that can disrupt the natural balance of bacteria in the vagina.
Some strategies for preventing BV include:
- Avoiding douching, which can disrupt the natural balance of bacteria in the vagina
- Limiting the number of sexual partners
- Using condoms during sexual activity to reduce the risk of sexually transmitted infections
- Avoiding the use of scented products in the genital area, such as soaps and sprays, which can irritate the vagina
- Wearing cotton underwear and avoiding tight-fitting clothing, which can trap moisture and promote the growth of bacteria
- Eating a healthy diet that includes probiotic-rich foods, such as yogurt and kefir, can help maintain the balance of vaginal bacteria
Women who are at high risk for BV, such as those with a history of the infection or those who are pregnant, may also benefit from the use of probiotic supplements or vaginal suppositories containing lactobacillus. These can help restore and maintain a healthy balance of bacteria in the vagina, reducing the risk of BV and other vaginal infections.
FAQ

Q: Can BV be sexually transmitted?
A: BV is not considered a sexually transmitted infection (STI), but having BV can increase the risk of contracting other STIs. However, sexual transmission of BV is not clear, as it can occur in women who have never had sex.
Q: Can men get BV?
A: BV is primarily a condition that affects women. While men can carry Gardnerella vaginalis, the bacteria commonly associated with BV, they do not typically develop symptoms of infection.
Q: Is BV contagious?
A: BV is not contagious in the sense that it cannot be spread through casual contact. However, sexual activity can increase the risk of developing BV or transmitting it to a sexual partner.
Q: Can BV affect pregnancy?
A: BV has been linked to several pregnancy complications, including preterm birth and low birth weight. Pregnant women with BV may be at higher risk of developing these complications and should seek prompt medical attention if they experience any symptoms of infection.
Q: Can BV go away on its own without treatment?
A: BV can sometimes resolve on its own without treatment, but it is important to seek medical attention if you experience any symptoms. Women without symptoms of BV but who are found to have Gardnerella vaginalis colonization do not need treatment.
Q: How long does it take to treat BV?
A: Treatment for BV typically involves a course of antibiotics taken orally or vaginally. The duration of treatment can vary but typically lasts 5 to 7 days.
Conclusion:
Bacterial vaginosis (BV) is a common condition that affects many women at some point in their lives. BV is caused by an imbalance in the vaginal flora, which can lead to symptoms such as abnormal vaginal discharge, vaginal odor, and vaginal irritation.
While BV is not typically considered a sexually transmitted infection, sexual activity can increase the risk of developing BV or transmitting it to a partner. Several risk factors can increase the likelihood of developing BV, including new or multiple sex partners, douching, and recent antibiotic use.
Treatment for BV is typically effective and involves a course of antibiotics, although the condition can recur after treatment. Prevention of BV involves maintaining good vaginal health and avoiding behaviors that can disrupt the natural balance of bacteria in the vagina.