The Human Immunodeficiency Virus (HIV) has been a topic of extensive research and discussion since its discovery. Its complexity and adaptability have made it a challenging adversary in the medical field. In this article, we’ll delve deep into the intricacies of HIV, breaking down its types, subtypes, groups, and strains. By the end, you’ll have a comprehensive understanding of this virus and its many facets.
HIV, or Human Immunodeficiency Virus, is a retrovirus responsible for causing AIDS (Acquired Immunodeficiency Syndrome). Before diving into its types and subtypes, it’s essential to grasp the basics of this virus and its impact on global health.
The Basics
HIV targets the immune system, specifically the CD4 cells (T cells), which help the immune system fight off infections. When left untreated, HIV reduces the number of CD4 cells in the body, making the person more likely to get infections or infection-related cancers.
- Transmission Methods:
- Unprotected sexual contact with an infected person.
- Sharing needles or syringes with someone who has HIV.
- Receiving contaminated blood products or organ transplants.
- From mother to child during childbirth or breastfeeding.
Global Impact
The global impact of HIV is profound, with millions affected worldwide. Despite advancements in treatment, the virus continues to be a significant public health issue, especially in low and middle-income countries.
- Statistics:
- As of 2020, approximately 38 million people worldwide were living with HIV.
- More than 36 million people have died from AIDS-related illnesses since the beginning of the epidemic.
- Sub-Saharan Africa remains the most severely affected region, with nearly 1 in every 25 adults living with HIV.
Types: 1 vs. 2
There are two main types of HIV: HIV-1 and HIV-2. While they share similarities, there are crucial differences between them, including their origins, prevalence, and response to treatments.
Origins and Characteristics of -1
HIV-1 is the most common and widespread type of HIV. It is believed to have originated from the transfer of the virus from chimpanzees to humans in Central Africa.
- Characteristics:
- Has a higher rate of transmission.
- Progresses more rapidly to AIDS without treatment.
- Divided into multiple groups and subtypes (which we’ll explore further in the next sections).
Origins and Characteristics of -2
HIV-2 is less common and primarily found in West Africa. It is believed to have originated from the transfer of the virus from sooty mangabey monkeys to humans.
- Characteristics:
- Has a slower progression to AIDS.
- Less infectious in the early stages compared to HIV-1.
- Has a longer asymptomatic stage.
Groups and Their Significance
Within the two primary types of HIV, there are distinct groups. These groups are essential to understand as they influence the virus’s behavior, transmission, and response to treatment.
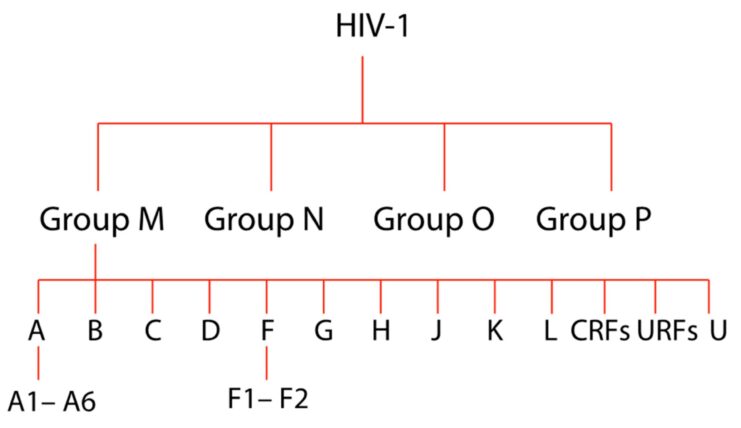
Groups of -1
HIV-1 can be divided into four groups: M (Main), O (Outlier), N (Non-M, Non-O), and P. Each group has a different origin and genetic makeup.
- Group M: This is the most common group, responsible for the majority of HIV infections worldwide.
- Originated from the transfer of the virus from chimpanzees.
- Contains several subtypes (A through K).
- Group O: Less common than Group M and primarily found in Cameroon and neighboring countries.
- Originated from western lowland gorillas.
- Less responsive to certain antiretroviral treatments.
Groups of -2
HIV-2 consists of two main groups: A and B. While both groups are primarily found in West Africa, Group A is more widespread and is the primary cause of the HIV-2 epidemic.
- Group A: More common and responsible for the majority of HIV-2 infections.
- Has a slower progression to AIDS compared to Group B.
- Less infectious in its early stages.
- Group B: Less common and found in specific regions of West Africa.
- Has a faster progression to AIDS compared to Group A.
- More infectious in its early stages.
Subtypes: A Kaleidoscope of Variations
HIV-1, particularly Group M, is further divided into subtypes. These subtypes are crucial to understand as they can influence the virus’s transmission, progression, and response to treatments.
Common Subtypes of – 1 Group M
Group M of HIV-1 consists of several subtypes, each with its unique genetic makeup and geographical distribution.
- Subtype A: Found in East and West Africa. It’s also seen in some parts of Asia.
- Known for its moderate transmission rate.
- Has a few circulating recombinant forms (CRFs) associated with it.
- Subtype B: Predominant in North America, Europe, Australia, and parts of South America.
- Most researched subtype due to its prevalence in the western world.
- Forms the basis for many HIV diagnostic tests and treatments.
Less Common Subtypes and Their Significance
While Subtypes A and B are more prevalent, other subtypes play a significant role in specific regions.
- Subtype C: Most common in Southern Africa, India, and parts of Brazil.
- Responsible for the majority of infections in India and South Africa.
- Known for its rapid transmission rate.
- Subtype D: Found mainly in East Africa.
- Has a faster progression to AIDS compared to other subtypes.
- Associated with higher mortality rates.
Recombinant Strains: When Subtypes Intersect
As it replicates, it can combine genetic material from different subtypes, leading to the formation of recombinant strains. These strains add another layer of complexity to the landscape.
Circulating Recombinant Forms (CRFs)
CRFs arise when an individual is infected with two different subtypes of the virus. The two strains can exchange genetic material, leading to a hybrid virus.
- CRF01_AE: A combination of subtypes A and E, prevalent in Southeast Asia.
- Associated with a rapid progression to AIDS.
- Has a high transmission rate.
- CRF02_AG: A mix of subtypes A and G, commonly found in West and Central Africa.
- Represents a significant portion of infections in these regions.
- Known for its moderate transmission rate.
Unique Recombinant Forms (URFs)
URFs are recombinant strains that are identified in a specific individual or a limited group of individuals.
- Significance of URFs:
- Indicate the ongoing evolution and adaptability of the virus.
- Highlight the importance of continuous monitoring and research to track new strains.
Strains: The Microscopic Differences
Beyond types, groups, and subtypes, HIV can be further classified into strains. These strains represent minor genetic variations within a subtype or group.
The Evolution of Strains
As the virus replicates, it can introduce small genetic mutations, leading to the emergence of different strains within a subtype.
- Factors influencing strain variations:
- The host’s immune response.
- The use of antiretroviral therapy.
- Other environmental and genetic factors.
Implications of Strain Differences
While the differences between strains might be minute, they can have significant implications.
- Drug Resistance: Some strains might develop resistance to specific antiretroviral drugs.
- This can complicate treatment plans and reduce the efficacy of certain medications.
- Disease Progression: Certain strains might be associated with faster or slower progression to AIDS.
- Understanding these differences can help in tailoring treatment and intervention strategies.
Treatment Implications Based on Variations
The diverse landscape of types, subtypes, and strains has significant implications for treatment. Tailoring antiretroviral therapy (ART) based on these variations can optimize outcomes for individuals living with.
Antiretroviral Therapy (ART) and Subtype Variations
The efficacy of certain antiretroviral drugs can vary based on the HIV subtype or strain an individual is infected with.
- Subtype-specific challenges:
- Some subtypes have inherent resistance to specific drugs.
- The rate of drug resistance development can vary between subtypes.
- Treatment regimens might need adjustments based on the prevalent subtype in a region.
Personalized Treatment Approaches
With advancements in genomics and personalized medicine, there’s a move towards tailoring HIV treatment based on an individual’s viral and genetic makeup.
- Benefits of personalized treatment:
- Optimized drug efficacy.
- Reduced side effects.
- Lower risk of developing drug-resistant strains.
Prevention Strategies: Beyond the Medical

While medical interventions are crucial, understanding the variations of HIV also underscores the importance of holistic prevention strategies that consider socio-cultural and economic factors.
Socio-cultural Implications of Variations
Different regions, with their dominant HIV subtypes or strains, might have unique socio-cultural factors influencing transmission.
- Factors to consider:
- Cultural norms around sexual health and relationships.
- Stigma associated with HIV testing and treatment.
- Access to education and awareness programs.
Economic Factors and Prevention
Economic stability can play a pivotal role in HIV prevention, especially in regions with high prevalence rates.
- Economic interventions:
- Improving access to healthcare services.
- Providing affordable antiretroviral drugs.
- Supporting community-based awareness and education programs.
FAQ
1. How is it different from AIDS?
HIV (Human Immunodeficiency Virus) is the virus that can lead to AIDS (Acquired Immunodeficiency Syndrome). While HIV is the virus that infects individuals, AIDS is the final stage of the infection when the immune system is severely damaged.
2. Can it be cured?
As of now, there is no cure for HIV. However, with proper medical care, HIV can be controlled, and individuals can lead healthy lives for many years.
3. How can one prevent transmission?
Preventive measures include practicing safe sex using condoms, not sharing needles, taking pre-exposure prophylaxis (PrEP) if at high risk, and ensuring safe blood transfusions.
4. Are there any side effects to medications?
Yes, like all medications, antiretroviral drugs can have side effects. These can range from mild issues like fatigue or nausea to more severe ones. It’s essential to discuss any side effects with a healthcare provider.
5. How often should one get tested for HIV?
The frequency of testing depends on individual risk factors. Those at higher risk, such as individuals with multiple sexual partners or those who inject drugs, should consider getting tested more frequently.
6. Can pregnant women with prevent transmission to their babies?
Yes, with proper medical care and treatment during pregnancy, the risk of transmitting HIV to the baby can be significantly reduced.
Final Thoughts:
The journey against HIV/AIDS is a collective one, filled with challenges, learnings, and moments of triumph. By understanding the virus in all its complexity and embracing a holistic approach, we inch closer to a world where HIV/AIDS is a thing of the past. Let’s continue the fight, armed with knowledge, compassion, and unity.
Related Posts:
- How To Tell If CPU Is Dead? Know All The Signs and Reasons
- 3 Male Body Types: Ectomorph, Mesomorph, Endomorph
- HIV ELISA Test And HIV ECLIA Test: The Power of Accuracy
- When to Test for HIV During and After Completion of…
- What is Anonymous HIV Testing? Peace, Privacy, and…
- MMM2 – HIV Screening and Diagnosis